Differential
expression of endothelial nutrient transporters (MCT1 and GLUT1) in the
developing eyes of mice
Ayuko Kishimoto, Hiromi Takashi-Iwanaga, Masahiko Watanbe M, Toshihiko
Iwanaga
The paper can be accessed here.
Introduction
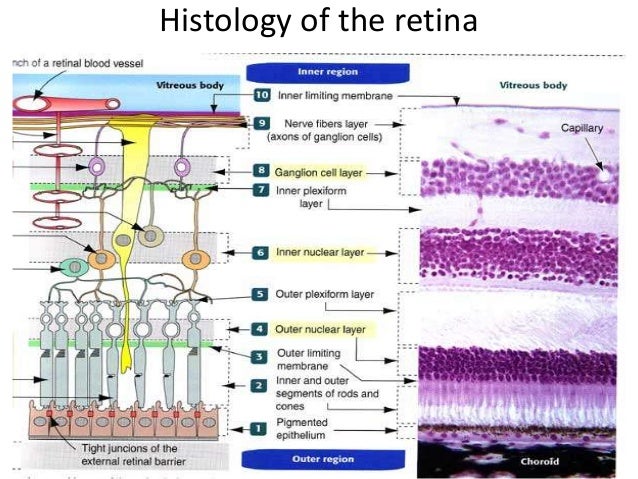
Endothelial cells at the blood brain express
glucose transporter (GLUT)-1 for uptake of glucose, but also express
monocarboxylate transporters (MCT), which are required because neonates depend
on monocarboxylates derived form milk as a source of energy. Within adults, all
blood tissue barriers, including the blood retina barrier, express both GLUT1
and MCT1.
During development, a special hyaloid vascular
system develops as part of the ocular vascular system, which degenerates during
later stages of development of the eye. The hyaloid artery branches into tunica
vasculosa lentis (TVL) at the lens and the vasa hyaloidea propria (VHP) along
the internal surface of the retina. In later stages of development, the hyaloid
artery, along with its branches regress, as the central artery and its six
branches develop to form the permanent vasculature of the eye supplying blood
to the inner two thirds of the retina. As within the central retinal artery, tight
junctions between the endothelial cells of the hyaloid artery limit diffusion
into the perivascular space. This results in the need of transporters such as
GLUT1 for transport of nutrient across the blood-retina barrier.
This study investigates the morphology of
ocular vessels expressing GLUT1/MCT1 to characterize the new development of
blood vessels differentially expressing GLUT1 and MCT1 in the eye.
Methods
Eye samples were obtained from embryos,
neonates of postnatal day 0-3, 5, 7, 9, 11, 13, 15, 20 and 25 as well as adult
mice. The retina and lens were isolated from these eyeballs.
Immunohistorchemistry was performed on samples, and to obtain double
immunoflourescnce, the samples were incubated with anti-MCT1 antibody,
ant-GLUT1 antibody and anti-CD31 antibody.
Silver intensified immunogold staining was
used for electron microscopy, where frozen sections were incubated with an
anti-MCT1 antibody followed by a secondary antibody covalently linked with gold
particles. Subsequently, the samples underwent silver enrichment and were
stained with uranyl acetate and lead citrate for observation under an electron
microscope.
For scanning electron microscopy, posterior
sections of the eyeballs and sections of the cerebral cortex were obtained,
prepared and coated with osmium in a plasma osmium coater. The samples were
then examined with and SEM at an acceleration voltage of 5kV.
Results
Hyaloid Vascular system
In fetuses, the VHP (on the surface of the
retina) and VTL (on the lens) of the hyaloid vascular system both possess GLUT1
transporters. The VHP had GLUT1 transporters running along the entire length,
with a few MCT1 expressing cells dispersed within the endothelium f neonates.
The frequency of MCT1 expressing cells was higher at the periphery of the
VHP. In the VTL, GLUT1 transporters were
present throughout, but MCT1 transporters were dispersed at the posterior and
lateral surfaces of the lens. The hyaloid vascular system, present only in
early stages of development, expressed GLUT1 along its entire length, whereas
retinal and brain endothelia predominantly express MCT1 in early stages of
development.
Fig. 6. An equatorial view of a lens stained for MCT1 and GLUT1. Some MCT1-expressing vessels intermingle with GLUT1-expressing vessels of the TVL. Bar 200 μm.
Vascular systems in the
developing retina
Vascularisation
of the retina begins at birth. Up to day 3, growing capillaries do not have
either GLUT1 or MCT1 transporters. Around postnatal day 5, MCT1 transporters
begin to appear in the retina near the optical disc and spread into the
superficial layer of the retina by till day 7. Neither GLUT1 nor MCT1 is
observed in the central retinal artery or any of its six branches. However, the
veins and capillaries both expressed MCT1. A dense sprouting, dense around the
vein but scarce around the artery, did not express MCT1 or GLUT1. The sprouting
began near the optic disc at day 0 and extended to t hora serata by day 9. During
angiogenesis, desmin (a component of muscle specific intermediate filaments)
was expressed in pericytes and the smooth muscles cells of the vessels. The pericytes
were found around MCT1 expressing central plexus. GLUT1 transporters increased
slowly in the ocular vessels after day 11, and at day 20 were comparable to the
frequency of MCT1 transporters. At day 25, the GLUT1 transporters appeared to
be more dominant than MCT1 transporters.
Radicular Projections
MCT1 expressing capillaries displayed long
projections of uniform thickness that did not branch dendritically. These were
not filopodia as the were around 5um in thickness, whereas filopodia are
thicker. These projections were not associated with pericytes and were seen
singly or in small groups all along the capillaries. These projections were
also seen around veins expressing MCT1 but not in arteries, which had no MCT1.
These projections were most dense on days 5 through 11, the mid-stage for
suckling, and were absent by day 20. These projections were also found in
capillaries of the neonatal brain.
Figure 12. Scanning electron micrographs of capillary vessels in the
retina at neonatal 7 days. The extracellular matrix has been thoroughly removed
by alkaline maceration to expose the surface of endothelial cells. Many
radicles project from the outer surface of endothelial cells (E). Bars
10 μm (a), 1 μm (b).
Discussion
The hyaloid vascular system initially only expressed
GLUT1, whereas retinal capillaries and veins expressed MCT1. This may be because
the hyaloid vasculature is a temporary vascular system. Also, MCT1 expressing
endothelial cells were present amidst GLUT1 expressing endothelial cells in
hyaloid vessels, indicating specific regulation of MCT1 and GLUT1 during
angiogenesis, a patter not observed in the brain.
Capillaries and veins of the developing
retina predominantly express MCT1, likely in response to the presence of
monocarboxylates from milk as a source of energy. Also, in the developing eye, the
shift from MCT1 to GLUT1 expression occurs after weaning. During angiogenesis,
arteries did not express any MCT1 or GLUT1.
The radicular projections observed in the SEM
were a surprising feature in this research. These were found in MCT1 expressing
cells in both the retina and the brain. These projections may indicate a novel
feature in vessel growth present in both retinal and brain endothelium and may
be related to the use of monocarboxyaltes as an energy source.
The overall findings showed that differential
expression of MCT1 and GLUT1 occurs in the ocular vasculature during
development. Some of these features observed in the blood-retinal barriers can
be seen in the blood-brain barrier as well. The presence of radicular
projections indicate a novel feature present in angiogenesis.
Critique
This paper was an easy read, with the introduction covering all the information required to understand the research. The layout was also easy to follow, and the text of the body as well as the figures were large enough to read. The figures were extremely clear with straightforward explanations. There was no unnecessary, excessive information in the paper, making it a simple read.
The research itself was very straightforward,
with three procedures. The paper explains development of vaculature in
the eye in an excellent way, describing all the vessels and arteries present during different developmental stages. It took into
consideration previous research on vasculature in the eye as well as energy
transporters present within the vasculature of both the eye and the brain.
Incorporating previous research into their paper, the authors were also able to
correct errors that arose in previous studies. A great component of the paper
is that the researchers came across a novel feature of the developing vessels
in the eye and brain whilst trying to understand development of blood vessels
in terms of expression of endothelial transporters. This novel feature gives the paper an edge in terms of possible future research.
The overall quality of this paper and
research is excellent. However, there were some issues in the paper. The
discussion mostly reiterates the results and does not expand on possible
reasons of why certain results were obtained or try to provide causative
information on their results. In addition, I think that the research should
have been conducted on the eyes at the first 30 postnatal days in order to
ensure complete understanding of developmental stages. Often times, the
researchers found that a process appeared sometime between to study dates, but
were not able to state the exact time of development. I believe that in a
developmental study it is important to know exact timing of each developmental
stage.
Whilst some aspects of the experimental
design and the material of the discussion may be lacking, the paper, in
general, does a wonderful job at investigating differential expression of
nutrient transporters in developing ocular vasculature and opens the door to
further research regarding endothelial development in the eye as well as the
brain.
References
Kishimoto A., Takashi-Iwanaga H., Watanabe M., Iwanaga T., 2016. Differential expression of endothelial nutrient transporters (MCT1 and GLUT1) in teh deloping eyes of mice. Experimental Eye Research. 153:170-177.
References
Kishimoto A., Takashi-Iwanaga H., Watanabe M., Iwanaga T., 2016. Differential expression of endothelial nutrient transporters (MCT1 and GLUT1) in teh deloping eyes of mice. Experimental Eye Research. 153:170-177.